Urate solubility in peripheral joints: Why 6.8?
Nicholas A Sumpter (1,2), Riku Takei (1), Mariana Urquiaga (1), Angelo Gaffo (1), Tony R. Merriman (1,3)
Affiliation(s):
1. Division of Clinical Immunology and Rheumatology, Department of Medicine, University of Alabama at Birmingham, Alabama, United States
Department of Internal Medicine, Radboud University Medical Center, Nijmegen, Netherlands
2. Department of Microbiology and Immunology, University of Otago, Dunedin, New Zealand
Objectives: We aimed to determine the appropriate definition of hyperuricemia based on urate solubility in peripheral joints. We then evaluated the implications of these results on appropriate target serum urate concentrations for urate lowering therapy.
Methodology: We reviewed published serum urate thresholds for hyperuricemia and their reported justifications. We then reviewed published data on intra-articular temperatures to identify the appropriate temperature to derive urate solubility. We then reproduced the results of Loeb (1972) using the data from Allen (1965) to calculate urate solubility at internal joint temperatures.
We also investigated publications of urate concentrations in the synovial fluid relative to the serum. Finally, we identified the serum urate concentration at which gout prevalence becomes apparent in the UK Biobank after excluding those on urate lowering therapy.
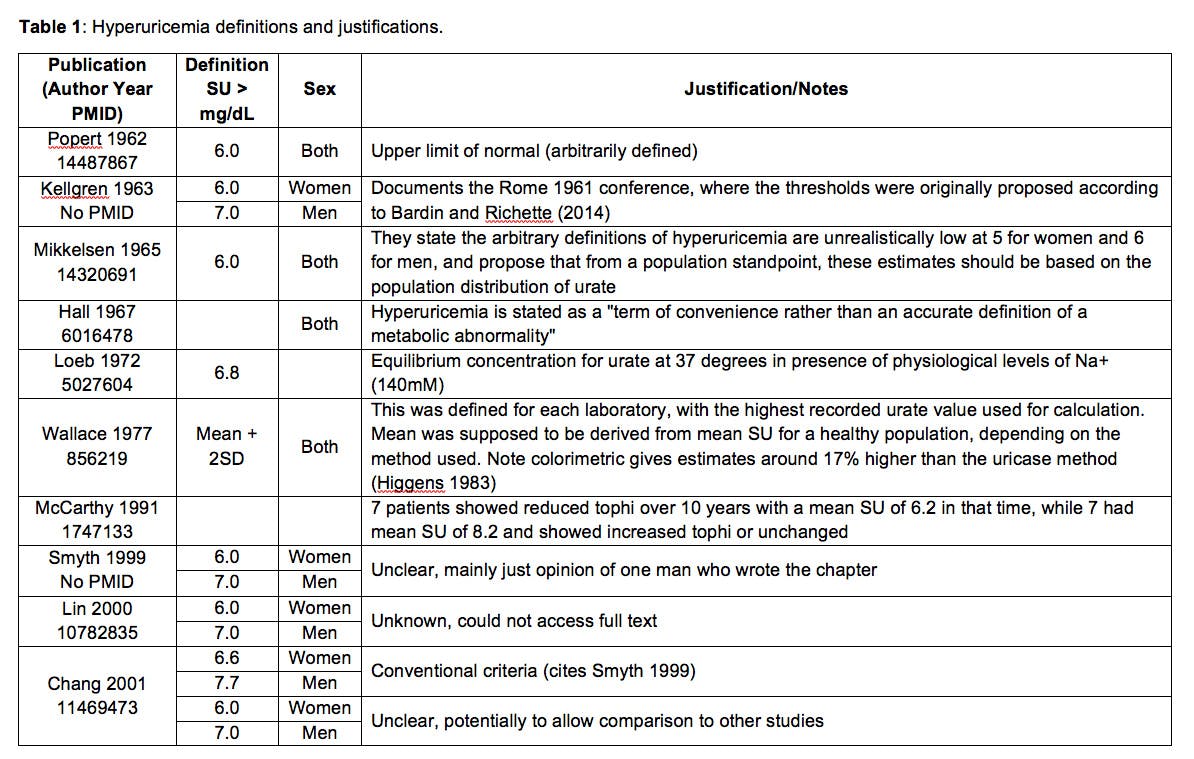
Findings: In the literature, hyperuricemia was variably defined as serum urate levels above thresholds of 5.7 to 10 mg/dL, typically between 6 and 7 mg/dL (Table 1). Where justifications were given, most publications arbitrarily defined hyperuricemia. In some cases the justification was related to urate solubility, suggesting that urate was saturated above the stated threshold, generally proposed to be 6.8 mg/dL based on Loeb (1972) and Allen (1965). In many studies different thresholds were proposed for men vs women.
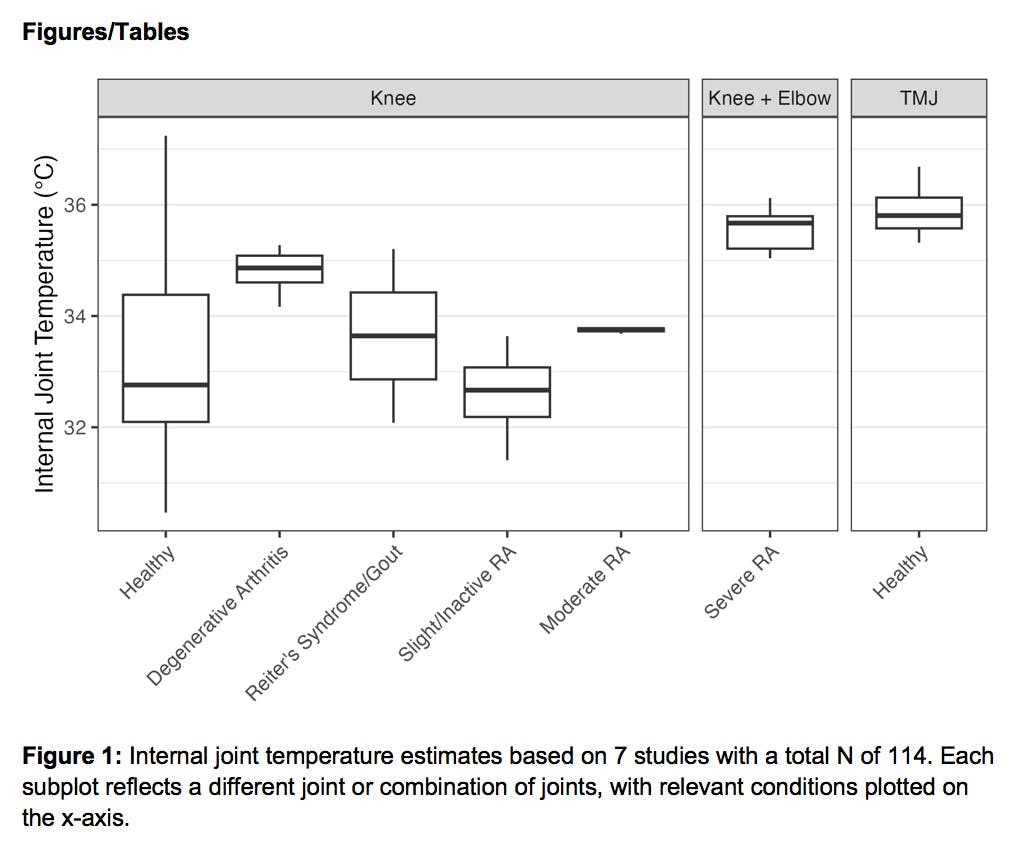
Intra-articular temperatures ranged from 29.7°C to 37°C, in most cases measured in the knee joint, with a mean of approximately 33°C among healthy individuals (Figure 1 & Table 2). At this temperature, the urate solubility threshold in the presence of physiological sodium levels (140mM) would be 5.3 mg/dL based on data from Allen (1965) and Loeb (1972) (Figure 2).
We identified 11 publications that largely showed ~10% lower synovial fluid urate concentrations vs serum in both healthy individuals and those with non-gout arthritides. However, this difference was reversed in those with gout, with ~10% higher synovial fluid urate concentrations vs serum.
We also found that gout prevalence becomes apparent above a serum urate concentration of approximately 6 mg/dL in both men and women of the UK Biobank cohort, exponentially increasing in prevalence at higher urate concentrations (Figure 3).
Significance: This study first showed that most hyperuricemia definitions are arbitrary. When based on urate solubility, a threshold of 6.8 mg/dL is likely inaccurate for peripheral joints, with a more accurate threshold being ~5 mg/dL. However, synovial fluid urate concentrations appear to differ from serum urate concentrations, and this difference is dependent on gout status. In gout cases, it may therefore be appropriate to reduce serum urate concentrations to below 4.5 mg/dL to result in a synovial fluid urate concentration below the urate solubility threshold. Estimates in the UK Biobank would suggest that serum urate concentrations of >6 mg/dL are required for gout to develop, with higher concentrations increasing gout risk exponentially, consistent with published results of incident gout in other cohorts.
The solubility threshold represents the point at which solid urate is in equilibrium with its dissolved form, therefore lower urate levels further encourage crystal dissolution and suppress crystal growth. Importantly, one should also consider sodium concentration, pH and other variables (e.g. proteins) that have also been implicated in urate crystallization.